What Is Heart Valve Disease?
Heart valve disease is common and serious, but treatable.

What are the types of heart valve disease?
Heart valve disease can occur in any of the heart's four valves, but certain types are more common than others.
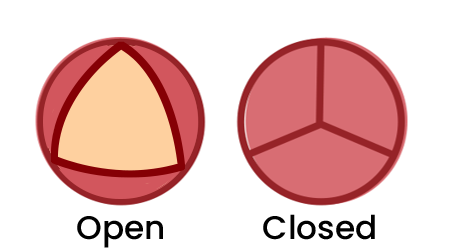
Normal aortic valve
The valve fully opens & closes
The valve doesn’t open enough
The valve doesn’t fully close & leaks
Learn more about specific conditions that impact the heart valves:

Symptoms
The symptoms of heart valve disease vary, depending on which valve is affected and how badly it has been damaged. Symptoms are not always obvious, even when valve disease is severe. And symptoms are often dismissed as a general sign of aging.
Here are the most common symptoms to watch for:
Fatigue or reduced exercise ability
Shortness of breath or fatigue after a previously normal amount of activity
Irregular heartbeat
Dizziness
Chest pain
Fainting
Ankle swelling

Detecting heart valve disease
Heart valve problems are often first detected during a routine medical exam when your healthcare provider listens to your heart with a stethoscope and hears an extra noise called a murmur.
A murmur does not necessarily mean you have heart valve disease. Depending on what your healthcare provider hears, you may be sent for further tests.
“Many people with heart valve disease have no symptoms, so it is important to have your heart listened to regularly.”
Heart murmur sounds
The heart has four valves that open and close to control blood flow to your body. If one or more of those valves don’t open or close properly, that means you have heart valve disease. It may be something you were born with, or that develops during your life.

Who is at risk?
Heart valve disease is usually caused by wear and tear, disease, or damage. The most common risk factors for valve disease are:
Older age - Wear and degeneration to the valves is the most common cause of valve disease. Degeneration is the slow breakdown of the leaflets and attachments and most commonly affects the mitral valve. It can also be caused by calcification—the gradual build-up of calcium that hardens and thickens on the valve and most commonly affects the aortic valve (aortic stenosis).
Congenital abnormalities - People can be born with narrow, deformed, or even missing valves. For example, around 1 – 2% of people are born with a bicuspid aortic valve that has two leaflets instead of the normal three, and that typically leads to valve disease.
Cardiovascular diseases and conditions - Problems with the heart or vascular system can also result in valve problems. For example, heart attacks can cause scarring of the heart muscle and distort the valves, an enlarged heart can stretch open a valve, long-term raised blood pressure can cause heart damage, and aortic dissections or tears can extend to the valve.
Family history - Blood relatives who had/have valve disease may increase risk.
Radiation to the chest and certain chemotherapy - Some types of cancer require radiation therapy to the chest that can damage the valves and cause valve disease many years later. Certain types of chemotherapy can also cause valve damage.
Other health conditions - Chronic kidney disease, lupus, and Marfan syndrome can all increase risk.
How does rheumatic fever lead to valve disease?
Rheumatic fever can cause lasting heart damage, including valve problems and heart failure. The mitral valve is most commonly affected; prolonged inflammation can weaken the muscles. The infection can cause the valve’s leaflets to stick together, narrowing the opening (mitral stenosis). The infection can also scar the valve, stopping it from fully closing, which allows blood to leak backwards (mitral regurgitation).

Diagnosing heart valve disease
If you have symptoms or if you have a murmur that doesn’t sound normal, your healthcare provider will arrange for further testing to diagnose the severity of your condition as well as to determine the best treatment options.
Expect to be booked for one or more of the following tests:
Electrocardiogram (ECG) to measure your heart’s electrical patterns
Echocardiogram to get sound wave images of your heart and valves
Chest x-ray to look for fluid in your lungs or enlargement of your heart
Cardiac magnetic resonance imaging (MRI) to create detailed images of your heart
Exercise or stress tests to see how the valves change or symptoms develop with exertion
Cardiac catheterization to examine blood flow and test how well the heart and valves are functioning
How serious is my condition?
Your doctor may describe your condition as mild, moderate or severe, based on the results of your tests.
If you have mild heart valve disease, you may not need to see a cardiologist straight after diagnosis. Your primary care provider will likely arrange a follow-up echocardiogram 12-18 months after your diagnosis to keep an eye on your heart valve function. Most people with mild heart valve disease can carry on with their daily activities. And, for a lot of people, the disease might not get worse.
If you have moderate heart valve disease, you may need more frequent follow up tests and check-ins with your healthcare provider. If you begin to experience new symptoms, your primary care provider may advise that you see a specialist.
If you are diagnosed with severe heart valve disease, you will be referred to see a cardiologist. Even if you are not experiencing any symptoms, you may need treatment to make sure your heart valve disease does not get worse.
Whether you have mild, moderate, or severe heart valve disease, it is important to have your heart checked regularly and to report any new symptoms immediately.

Treatments for heart valve disease
Treatments for heart valve disease are based on many factors, including the severity and symptoms, how well your heart is functioning and your overall health.
Your healthcare provider should carefully explain the risks and benefits of each approach for you. Together, you and your healthcare provider can make the best decision about the right treatment for you.
Treatment options may include:
Surgical valve replacement
Transcatheter-based valve replacement
Surgical valve repair
Transcatheter-based valve repair
Medical management
Heart valve surgery
There are two main types of heart valve surgery.
Valve repair is most often used to repair the mitral valve when it is not closing properly, although, in some cases, other valves can also be repaired.
Valve replacement is when the diseased valve is replaced with another valve. This is most common with the aortic valve.
There are two main types of replacement valves: mechanical valves (made of ultra smooth carbon) and tissue valves (animal or synthetic).
-
Minimally invasive surgery
Some types of valve replacements can be done using minimally invasive surgery. Minimally invasive means, the surgeon does not cut through the breastbone. Instead, the valve is replaced using special equipment, including very small cameras inserted through one or more small cuts in the skin on the chest. Minimally invasive surgery may reduce your level of discomfort after the operation but depending on the valve and other factors, it may not always be possible.
-
Transcatheter treatment
A transcatheter procedure is a type of minimally invasive surgery that uses a catheter (a thin, flexible tube) to access the damaged heart valve. Transcatheter procedures are less invasive than open-heart surgery and have shorter recovery times. There are different types of transcatheter procedures, depending on which valve is affected.
-
Valvuloplasty
Valvuloplasty is a rare treatment for heart valve disease. It is used to treat valve stenosis. Valvuloplasty is done during a procedure called cardiac catheterization. The cardiologist inserts a soft, thin tube called a catheter tipped with a balloon into a blood vessel, usually in the groin. The catheter is carefully guided to the narrowed valve in the heart. Once in position, the balloon is inflated to widen the valve, improving blood flow. The balloon is then deflated, and the catheter with the balloon is removed.
-
Surgical valve replacement
A surgical valve replacement is usually performed by open heart surgery or, if possible, minimally invasive surgery with smaller incisions. A surgeon can replace a valve with either a mechanical valve or a biological valve. Both types have benefits and drawbacks:
Mechanical valves are made of carbon or metal and are very durable. This means they do not wear out, but they require you to take blood thinners and can sometimes produce an audible clicking noise.
Biological valves are made of animal tissue that is strong and flexible enough to last 10-20 years. They don’t require you to take blood thinners, but they do need to be replaced if they wear out.
-
Surgical valve repair
How a valve is repaired depends on the specifics of what needs to be fixed. This can range from clearing away calcium build-up, separating parts of the valve that didn’t properly separate, or reshaping the mouth of the valve so that all parts can properly connect
-
Transcatheter-based valve repair
This involves a thin tube, called a catheter being inserted through a blood vessel, giving access to the heart valve to insert devices to bring the edges of the valve together. This helps the valve close more completely, reducing regurgitation (back flow from leaky valves).
-
Transcatheter-based valve replacement
This involves a thin tube, called a catheter being inserted through a blood vessel, giving access to the heart valve. A new biological valve can then be inserted without removing the original one. This treatment is preferred when open heart surgery is not appropriate.
-
Medical management
Body: Regular check-ups will be part of treating mild and moderate heart valve disease before it can become severe. You may be prescribed medications to relieve your symptoms, reduce complications, and/or manage risk factors. Although they can help to manage your symptoms, medicines are not a cure for heart valve disease.
-
Lifestyle Changes
With all heart valve diseases, healthy habits can improve your health generally and reduce the strain on your heart from everyday activities. Maintaining a healthy weight, stopping smoking, and starting light exercise like walking can help your heart adapt to work better despite valve disease.
Shared decision-making resource
The specifics of any heart valve disease treatment are unique to the disease and your individual circumstances. These resources will help you ask the right questions and participate in shared decision-making with your healthcare provider.

Frequently asked questions
Is heart valve disease genetic?
Some types of heart valve disease can be inherited. The most common is bicuspid aortic valve however, most forms of heart valve disease have more to do with natural aging and lifestyle than with your genes.
If one of your parents or other close family members has valve disease, it is important to share that information with your primary healthcare provider.
How serious is my heart valve condition?
Will I need to restrict physical activity after my valve replacement?
Does pregnancy affect my heart valve condition?
Does heart valve disease always require surgery?
No. Many Canadians who are diagnosed with heart valve disease can live a normal life with lifestyle changes and minimal treatment. Mild and moderate heart valve conditions may never need surgery. Regular check-ups help identify when heart valve disease is worsening and give you time to consider treatment options.
If I have no symptoms, does that mean my heart valve disease is mild?
No. You can have severe valve disease and feel fine. That’s why it is important to have a healthcare provider to assess your heart regularly.
Why do I need to see my dentist before heart surgery?
Having your teeth and gums checked reduces the risk of infective endocarditis, an infection that can enter your bloodstream and travel to your heart.
Gum disease (sometimes called gingivitis) is an inflammation that can lead to red and swollen gums that often bleed during tooth brushing. When the gums are inflamed and bleeding, it is easy for bacteria in the mouth to enter the bloodstream and cause infection. Individuals with heart valve disease are at higher risk for developing infective endocarditis, which is serious and, if not treated, can be fatal. Some hospitals won't proceed with your surgery unless you see a dentist, so it is important to take this seriously.