Aortic stenosis
What is aortic stenosis?
Aortic stenosis is when the aortic valve of the heart is narrow or stiff (calcified) and doesn’t fully open. This decrease in the opening of the valve makes it hard for blood to get out of the heart and to the rest of the body. This can weaken the heart over time and your body may not get the oxygen it needs; it can also cause fluid to back up into the lungs. Aortic stenosis can be mild, but may become more severe over time.
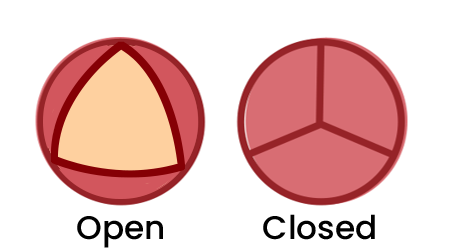
Normal aortic valve
The valve fully opens & closes
Aortic stenosis
The valve doesn’t open enough
Causes
Over a lifetime, the tissue in your heart valves becomes thicker and stiff (calcified) due to degeneration of the valve. For some people, the tissue thickening is greater and that can lead to aortic stenosis. As a valve’s tissue thickens, it can have difficulty opening fully. Causes that contribute to tissue thickening include:
Calcium buildup on the valve
Infection (e.g. rheumatic fever)
Congenital heart defects: Some people are born with a bicuspid aortic valve which means the valve only has two leaflets (cusps) instead of the normal three. This makes the heart work harder, causing it to “age” faster and potentially develop aortic stenosis earlier in life.
Symptoms
Early symptoms of aortic stenosis may be difficult to recognize because they are often dismissed as general signs of aging. Common symptoms include:
Shortness of breath or fatigue
Chest pain; especially with activity
Difficulty sleeping, or needing to sleep sitting up
Dry cough
As the stenosis gets worse, the symptoms become more serious and include:
Dizziness or fainting
Irregular heartbeat
If you have aortic stenosis, it’s important to monitor your symptoms using a symptom tracker and report changes to your healthcare provider. It’s also important to attend regular health checkups.

Treatments
If your valve requires treatment, a range of options may be available. Your heart team should carefully explain the risks and benefits of each approach for you. Together, you and your heart team can make the best decision about the right treatment for you. Treatment options may include:
Surgical aortic valve replacement (SAVR)
A surgical valve replacement is usually performed by open heart surgery or, if possible, minimally invasive surgery with smaller incisions. The surgeon removes the aortic valve and replaces it with either a mechanical valve or a tissue valve, which is sometimes called a bioprosthetic or biological valve.
When deciding which valve is right for you, here are some factors to consider:
Mechanical valves are made of carbon or metal and are very durable – they can last a lifetime. This means it is less likely that you will need a second valve replacement.
With a mechanical valve, you will need to take blood-thinning medications every day for the rest of your life, to reduce the risk of blood clots forming in the valve.
Blood thinners increase your risk of bleeding which is important if some of your daily activities, such as your job or hobbies, increase your risk of falls, bumps or bruises.
Mechanical valves may make a clicking sound that you may be able to hear.
Bioprosthetic valve replacements are made of animal tissue that is strong and flexible enough to last 10-20 years.
They usually don’t require high doses of long-term blood-thinning medications which means your risk of bleeding is lower.
There is a higher chance you may need another operation with a bioprosthetic valve.
Catheter-based approach: Transcatheter aortic valve implantation (TAVI)
The TAVI procedure allows an aortic valve to be implanted using a long narrow tube called a catheter. Usually, the catheter is inserted into a large blood vessel in your groin and a new biological valve can then be implanted over the original one.
Catheter-based approaches are typically recommended when surgery is not appropriate. TAVI is recommended for people over 75, who have a higher risk associated with surgery. Complications, such as the need for a pacemaker implantation or problems with the valve leaking, are more likely with TAVI than with surgery.
Ross procedure
The Ross procedure is a specialized procedure for younger and active patients. This procedure replaces the aortic valve with the pulmonary valve. A donor valve (cadaveric homograft) is used to replace the original pulmonary valve. This requires a two-valve follow-up, but results in excellent life expectancy and quality of life. This procedure requires surgeons with specialized experience.
Lifestyle changes
With all heart valve diseases, healthy habits can improve your health generally and reduce the strain on your heart from everyday activities. Maintaining a healthy weight, stopping smoking, and starting light exercise like walking can help your heart adapt to work better despite valve disease.
Medical management
Regular checkups to monitor your heart health.
Your heart team may prescribe medications to relieve your symptoms, reduce complications and/or manage risk factors. Medicines are not a cure for heart valve disease.
Consider getting a blood test for Lp(a), a protein in your blood that can affect your risk of aortic stenosis.
There is a lot to consider when deciding on treatment. These resources will help you ask the right questions and participate in decision making with your heart team.
Patient Stories
If you have been diagnosed with aortic stenosis, you are not alone. Learn from people who share their experience — and what they learned about diagnosis, treatment and recovery.

Frequently asked questions
How will I know if my valve disease is getting worse?
Symptoms that indicate your valve disease is getting worse may not happen for years after you are diagnosed with a valve problem. The most common symptoms include feeling more tired than usual or getting short of breath during routine activities. You may experience swelling of your ankles and feet. You may also feel dizzy.
Often times, symptoms start to occur very gradually and, therefore, it’s a good idea to keep track and write them down when they occur. Tracking your symptoms is tracking your health! Use our downloadable and printable Symptom Tracker to capture your symptoms on a daily basis and bring your Symptom Tracker for all of your appointments with your health care provider so that together, you can make appropriate decisions about your care. If you start experiencing any of the symptoms above, see your doctor.
Send us your questions and we will try to answer as many as we can in upcoming editions of this newsletter.
What are the risk factors for aortic stenosis?
Risk factors for aortic stenosis include general wear due to aging, congenital heart defects, kidney disease, diabetes, high blood pressure, high cholesterol, previous infections present in the heart, and exposure to radiation therapy to the chest. It’s important to tell your healthcare practitioner if any of these risk factors apply to you.
I have severe aortic stenosis with no symptoms. When should I expect treatment?
Cases like yours have usually been managed with “watchful waiting” — regular cardiologist checks until symptoms appear or you meet criteria for treatment. But recent studies suggest that earlier treatment improves outcomes in some cases. Learn more.
Will aortic stenosis always need surgery?
Following my valve replacement surgery, I experienced what I can best describe as brain fog and reduced mental sharpness during my recovery. Is this common?
Postperfusion syndrome, often called "pumphead," is a set of brain problems that can happen after heart surgery when a machine, called a heart-lung bypass machine, is used to help pump blood through the body. The issues include problems with paying attention, focusing, remembering things for a short time, and making small movements with your hands. It might also take longer to think and move. These problems are usually temporary, with no lasting damage to the brain. If you have concerns, speak to your healthcare provider.
Is heart valve disease genetic?
Some types of heart valve disease can be inherited. The most common is bicuspid aortic valve however, most forms of heart valve disease have more to do with natural aging and lifestyle than with your genes.
If one of your parents or other close family members has valve disease, it is important to share that information with your primary healthcare provider.
I am considering a mechanical valve replacement and understand that I will need to take anticoagulants (blood thinners) for the rest of my life. What should I know before getting a mechanical heart valve?

Resources
Initial Consultation Guide
This guide will help you prepare for an appointment with your doctor and support an efficient, informative, and helpful consultation. It outlines the types of questions your doctor may ask you during the consultation, as well as questions you'll want to consider asking.
Shared decision making
People diagnosed with heart valve disease are often confronted with a wide range of treatment options. Shared decision-making involves doctors and patients working together to choose the most suitable treatment, based on the patient’s preferences and goals as well as clinical evidence and the care team’s expertise. These resources aim to support people with heart valve disease in participating in decision-making about their care.
Get the shared-decision making guide
Symptom Tracker
Our symptom tracker has been developed to help people who think they may have heart valve disease, or other cardiac conditions, prior to or during consultation periods with their doctor. It captures symptoms to help you and your doctor understand your health and assist with diagnosis and ongoing care planning.
Good news on non-surgical valve replacement for aortic stenosis
Trans-catheter aortic valve implantation (TAVI) has been in use for more than 20 years for aortic stenosis. So what have we learned about its outcomes, compared to open-heart valve replacement surgery? A review of clinical trials shows excellent results and allays concerns that the prosthetic valves used in TAVI could be less durable than those used in surgery.
A review of clinical trials shows excellent results for both non-surgical and surgical treatments for aortic stenosis, allaying concerns about the durability of the prosthetic valves used in TAVI (trans-catheter aortic valve implantation, a non-surgical treatment option).

There is life after treatment.
Each person’s path to recovery will look different. Your treatment plan will be unique to your needs, and likewise, your recovery — the time it takes to return to a normal activity level and adapt to lifestyle changes — may vary from what others experience. Taking time to recover, both physically and mentally, is an important part of your journey.